Have you ever felt like something happened in your life that you just can’t move past, no matter how much time goes by? Emotional trauma can feel exactly like that—something invisible yet profoundly powerful, lingering under the surface, impacting your emotions, relationships, and even your body.
We’ll dive deep into the heart of emotional trauma, explore what it truly means, why it sticks around, and how it shapes your everyday life. Because understanding it deeply is the first step toward feeling better, stronger, and eventually, freer.
What Exactly is Emotional Trauma?
We often imagine trauma as something dramatic—big, obvious events that only happen to others. But emotional trauma is quieter and much closer to home. It can arise from experiences you might dismiss or overlook, yet still profoundly affect your everyday life.
At its simplest, trauma is defined by the American Psychological Association (APA) as “the emotional response to an extremely negative event.” But what makes trauma truly impactful isn’t just the event itself—it’s how deeply your brain and body internalize and respond to that experience. It’s an emotional wound, invisible yet real, rooted in how your nervous system perceives safety and threat.
Consider trauma like an internal bruise. On the outside, everything might look fine. Inside, however, there’s tenderness, discomfort, or pain. Trauma is similar—a hidden injury that influences your reactions, decisions, and relationships, often without you realizing why.
Understanding trauma isn’t about labeling yourself but recognizing that certain experiences have genuinely shaped your emotional landscape—and that this shaping can be reshaped through healing.
How Does Emotional Trauma Change Your Brain and Body?
When trauma hits, your brain undergoes significant internal shifts, literally rewiring itself in response to extreme stress. Here’s what happens:
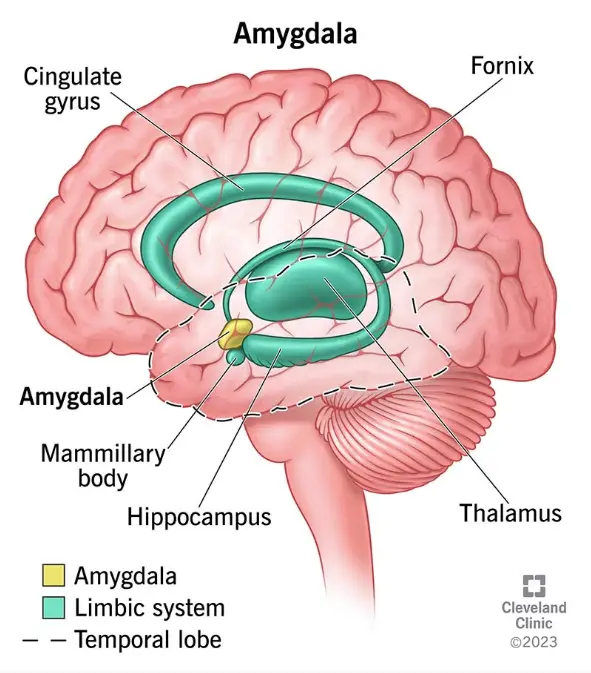
- Your Amygdala Goes on High Alert: Think of your amygdala—the brain’s fear center—as an overzealous security guard. After trauma, it’s always on duty, scanning your environment for threats, even in safe, everyday situations. This explains why seemingly minor triggers can send your anxiety skyrocketing.
- Your Prefrontal Cortex Takes a Backseat: The prefrontal cortex is your rational, logical friend who usually keeps things calm and balanced. During trauma, however, this part of the brain gets overwhelmed and temporarily steps back. Decision-making and emotional regulation become a struggle, making you feel like your emotions are out of your control.
- Your Hippocampus Gets Disrupted: The hippocampus handles memory and learning, and trauma floods this area with stress hormones, impairing its function. That’s why your memories of traumatic events might feel fragmented or incomplete, as if you’re trying to piece together a puzzle with missing pieces.
On a physical level, trauma doesn’t just stay “in your head”:
- Your Body’s Stress System Gets Overwhelmed: Chronic trauma disrupts your body’s normal stress-response system (known as the HPA axis). Instead of calming down after a stressful event, your body stays on high alert, continuously pumping stress hormones like cortisol. This prolonged stress can lead to physical issues such as chronic fatigue, inflammation, digestive problems, and insomnia.
- Trauma Can Even Affect Your Genes: Recent research shows trauma might impact your genetic expression (epigenetics). It can literally leave biological markers that influence how your body responds to stress, potentially affecting your physical and mental health long-term, and even extending to future generations.
The silver lining here is the concept of neuroplasticity: the brain can change and heal. The same way trauma changed the brain, positive experiences and therapies can help re-wire it again toward safety. In fact, the brain is constantly updating its predictions. With the right interventions, you can gradually teach your brain and body that the danger has passed, and they can regain a sense of calm and control. Healing is very much a mind-body process – involving calming the nervous system, strengthening the “thinking” brain, and releasing the tension stored in the body.
To better navigate your healing journey, let’s explore the different types of emotional trauma and their unique impacts.
Types of Emotional Trauma
Just as wounds come in different forms, trauma isn’t one-size-fits-all. Experts classify trauma in a few key ways. One basic distinction is between physical trauma (bodily injury) and emotional or psychological trauma (the emotional injury). Let’s break down some key types:
- Acute trauma – resulting from a single distressing event. For example, a serious car accident or a one-time assault might cause acute trauma. It’s the intense shock during or shortly after an isolated event.
- Chronic trauma – resulting from prolonged or repeated events, such as ongoing abuse, neglect, or violence over months or years. People in this situation endure high stress for an extended period. Complex trauma is a related term describing exposure to multiple traumatic events, often of different types, especially in childhood.
- “Big T” vs. “little t” trauma – a more informal way to recognize that not all traumas are obvious. “Big T” traumas are large, life-threatening events (natural disasters, war, major accidents) that anyone would recognize as traumatic. “Little t” traumas are smaller or less evident hurts (chronic humiliation, emotional neglect, childhood bullying). As Dr. Gabor Maté cleverly clarifies, “Big T traumas shout; little t traumas whisper. Both can leave you feeling like you’re stuck between stations, never quite catching the signal of safety.” In other words, even subtle, repeated hurts can accumulate and profoundly affect one’s sense of security.
- Secondary or vicarious trauma – trauma doesn’t always come from firsthand experience. Witnessing violence or even hearing about traumatic events happening to loved ones can traumatize someone. For instance, a child who witnesses domestic violence, or a first responder repeatedly encountering others’ trauma, may develop their own traumatic stress. Events you hear about or see from a distance can still leave a mark.
- Developmental trauma – trauma that occurs in childhood, especially repeated maltreatment or attachment trauma (like abuse or neglect by caregivers). This often leads to complex effects on personality and development, since the brain and sense of self are still forming.
Trauma is deeply personal and subjective. What might seem minor to one person could be profoundly traumatic to another. There’s no shame in how trauma impacts you—it’s simply your brain and body’s way of reacting to overwhelming stress.
Understanding these different forms of trauma helps you recognize your experiences better, and importantly, begin the journey of healing tailored specifically to your needs
Symptoms & Manifestations of Emotional Trauma
How do you know if someone (or yourself) is carrying an emotional trauma? Trauma can manifest in a wide range of symptoms, touching nearly every aspect of a person’s being – emotions, body, mind, and relationships. Often these symptoms don’t show up immediately; they might emerge days, months, or even years after the traumatic experience. Here are some common ways emotional trauma can show itself:
Emotional & Psychological Symptoms:
- Intense anxiety or constant fear
- Sudden anger or irritability
- Deep sadness, grief, or feelings of hopelessness
- Persistent guilt, shame, or self-blame
- Dissociation—feeling numb, detached, or outside your body
- Mood swings and emotional unpredictability
- Social withdrawal and difficulty trusting others
- Flashbacks or emotional reactions without clear triggers
Physical Symptoms:
- Chronic fatigue or exhaustion
- Sleep disturbances like insomnia or nightmares
- Muscle tension and heightened startle responses
- Unexplained aches, pains, or headaches
- Digestive issues and a racing heart
- Panic attacks or sudden anxiety episodes
- Feeling disconnected or numb physically
In day-to-day life, these symptoms can make it hard to function. You might notice someone with trauma being hypervigilant – always scanning their surroundings for threats, preferring to sit near exits, or being jumpy in crowds. They may avoid anything that reminds them of the trauma, which can constrict their life. For example, a car accident victim might avoid driving, or someone hurt in a past relationship might shut down emotionally with new people. Emotions can also “time-travel”: a harmless comment or a specific smell might trigger intense fear or shame in a trauma survivor because it unconsciously reminds them of the past.
Recognizing these trauma responses as normal reactions to abnormal events helps you approach yourself with compassion—understanding that trauma symptoms aren’t flaws, but natural protective responses to distress.
Emotional Trauma Risk & Resilience Factors
Trauma doesn’t play fair. Ever noticed how two people can go through something equally awful—like a breakup, a betrayal, or a major loss—and end up in totally different emotional places? One person starts putting the pieces back together. The other feels like they’re still crawling through emotional quicksand, wondering why it’s taking so long to “get over it.” Spoiler: it’s not about who’s stronger. It’s about what tools, support, and internal wiring each person had to begin with.
Let’s start with the tough stuff: risk factors. These are like invisible backpacks full of bricks you didn’t ask to carry. Trauma that hits early—especially if it repeats or comes from someone you were supposed to feel safe with—has a way of sticking to your nervous system like glue. It can shape your brain and body in ways that make healing feel like a game you weren’t given the rules for. One way it might show up? PTSD (Post Traumatic Stress Disorder). Not just feeling sad or shaken. We’re talking nightmares, panic attacks, a body that reacts as if you’re still in danger when you’re just, say, standing in line at the grocery store. Add in a history of anxiety, no support network, or back-to-back hard times, and yeah—your system might feel like it’s permanently stuck in “survival mode.”
But—and this is a big but—there’s another side to the story: resilience factors. These are your emotional shock absorbers. They’re the things that don’t erase trauma, but help you bounce a little, instead of shatter. The most powerful one? People. Just one person who sees you, hears you, and believes you can be enough to shift the weight. It might be a friend, a therapist, or even a stranger online who said the right thing at the right moment. Support matters more than we give it credit for.
Other ingredients for resilience? Feeling physically safe, having a few grounding routines, and being able to laugh—even if it’s through tears. Having access to your own self-soothing tools (yoga, playlists, comfort food, walks with your dog) is another big one. These aren’t just “nice-to-haves.” They’re the lifelines that help you feel like you’re not drowning.
And here’s a bit of underrated magic: resilience is teachable. It’s not reserved for the lucky or the zen. You can build it, slowly, awkwardly, and imperfectly. Psychologist Ann Masten calls this kind of resilience “ordinary magic.” And it really is—like finding calm in your breath, laughing with a friend, or realizing you’ve survived every hard day so far.
So, if you’ve been beating yourself up with questions like, “Why is this so hard for me?” or “Why am I still not over it?”—please, cut yourself some slack. Healing isn’t a race. It’s a deeply personal path with a lot of potholes. And the more we understand the mix of what holds us back and what lifts us up, the better we get at moving forward—even if it’s just one wobbly step at a time.
Conditions Related to Emotional Trauma
Here’s the thing, trauma doesn’t just come in, wreck your nervous system, and leave. It tends to leave souvenirs. And often, they show up in the form of other mental health struggles.
Let’s start with the big one: PTSD, or post-traumatic stress disorder. We’ve touched on this, but to go a little deeper—PTSD isn’t just about having a bad memory. It’s a full-body, full-mind experience. Flashbacks. Nightmares. That “always on edge” feeling, like your body never got the memo that it’s safe now. It makes you avoid people, places, or situations that remind you of the trauma. Sometimes even thinking about it feels impossible.
Then there’s C-PTSD, or Complex PTSD. That’s what happens when the trauma is long-term—often starting in childhood or happening in close relationships. On top of all the usual PTSD stuff, it throws in emotional numbness, intense shame, difficulty with trust, and a very shaky sense of self-worth.
But PTSD and C-PTSD aren’t the only guests at this party. Trauma has a way of inviting friends. Depression and anxiety are two of the most common. It makes sense—if your brain is constantly bracing for impact, joy becomes harder to access, and everyday worries can spiral quickly. Then there’s addiction—alcohol, drugs, food, even work or relationships—as ways people try to quiet the internal noise or escape the pain, even if just for a little while.
Dr. Bessel van der Kolk once said, “Not all addictions are caused by trauma, but all trauma can lead to addiction.” That line hits. Because for many, the coping starts as survival—but eventually becomes its own problem.
You might also see trauma show up in eating disorders, self-harm, or dissociation—that out-of-body, foggy, disconnected feeling that’s hard to explain but all too real. In severe cases, it can contribute to dissociative disorders, like DID (Dissociative Identity Disorder), often rooted in repeated early trauma.
And let’s not ignore the physical ripple effects. Chronic pain. Autoimmune conditions. Gut issues. Sleep problems. Trauma doesn’t just haunt the mind—it lingers in the body, too. As Gabor Maté puts it: the body holds what the mind can’t process.
Now, if you’re reading this and seeing yourself in a few places—take a breath. This isn’t about giving you a diagnosis or another label. It’s about helping you see the full picture. Because when trauma is part of the story, it often explains what nothing else has been able to.
And here’s the empowering part: when we start to heal trauma, many of those other struggles begin to soften, too. That’s why many therapists now use a trauma-informed approach—because healing the root can change everything. If traditional treatments haven’t worked, maybe it’s not you. Maybe they just weren’t looking in the right place.
So if you’ve ever felt like your symptoms don’t make sense, or like you’re a mess no one can untangle—this is your gentle reminder: there is a reason, and there is a way through it. And healing doesn’t mean fixing everything overnight. It means understanding yourself enough to stop blaming your struggle—and start meeting it with compassion.
Emotional Truama Recovery & Moving Forward

Healing from emotional trauma is absolutely possible—but it takes time. Think of it less like a race and more like rebuilding a house, one brick at a time. Here are some key paths that support recovery:
- Therapy is often the first stop, and for good reason. Trauma-focused approaches like CBT (cognitive behavioral therapy), EMDR (eye movement desensitization and reprocessing), somatic therapy, or psychodynamic therapy help unpack difficult memories, shift harmful beliefs, and regulate the nervous system. A good trauma therapist will always start by helping you feel safe—before diving into the hard stuff.
- Medications such as SSRIs, SNRIs and Prazosin can be helpful, especially when symptoms like anxiety, panic, or insomnia are making daily life hard to manage. These don’t “fix” trauma, but they can create a steadier foundation.
- Holistic practices—like yoga, mindfulness, tai chi, or creative expression—can offer powerful ways to reconnect with your body and emotions. When talking isn’t enough, movement and creativity can help process pain stored in the body.
- Support networks are critical. Whether it’s a close friend, a therapist, or a group of people who’ve been through similar experiences, human connection helps us feel safe, seen, and less alone. Trauma disconnects—support helps us reconnect.
- Emerging therapies like MDMA-assisted therapy (currently in trials) are showing promise for those who haven’t found relief through traditional approaches. The field of trauma healing is constantly growing.
Remember, healing takes time—and the process won’t always feel linear. Some days will bring progress, others might feel like you’re slipping backwards. But that’s all part of it. What matters most is how you meet yourself along the way. Self-compassion is what holds it together—the steady voice reminding you to celebrate the small wins, to speak gently to yourself, and to remember: healing isn’t about perfection. It’s about slowly finding your way back to who you’ve always been.
What About Growth After Emotional Trauma?
It might sound surprising, but for some people, healing doesn’t just mean getting back to baseline—it means growing in ways they never expected. This is known as Post-Traumatic Growth (PTG).
PTG doesn’t mean the trauma was good. It means that through the process of healing, some people discover:
- A stronger sense of self or personal strength
- Deeper appreciation for life and its everyday moments
- More meaningful relationships
- A shift in priorities or life direction
- Greater compassion or empathy for others
- Newfound purpose or spiritual connection
Growth often coexists with pain—it’s not one or the other. It’s the insight that says: “That was devastating, and yet—I found something in myself I didn’t know was there.”
You don’t have to aim for growth. Sometimes surviving is the win. But if, one day, you notice yourself thinking more deeply, loving more honestly, or choosing more boldly—know that’s growth, too. And it counts.
You don’t have to do it all at once. And you definitely don’t have to do it alone. Keep going—at your pace, in your way. That’s more than enough.
Conclusion
Emotional trauma has a way of turning life upside down. It can leave you feeling disoriented, disconnected, or like the world no longer fits. But if there’s one message worth repeating, it’s this: healing is not only possible—it’s real, and it’s already begun the moment you decided to understand what’s been happening inside you.
You may carry wounds that no one else can see, but that doesn’t make your pain any less valid—or your strength any less real. The fact that you’re here, reading this, tells a story of resilience. You don’t need to have it all figured out. You just need to keep showing up—for yourself, in small, kind ways.
Recovery isn’t about erasing the past. It’s about learning how to live in the present without being ruled by it. And it’s about building a future that isn’t defined by what hurt you, but by what you choose next.
So if today is a hard day, be gentle. If tomorrow feels lighter, let it be a reminder that more light is possible. Whether your next step is therapy, reaching out to someone you trust, or simply getting through the day—that step matters.
You’re not broken. You’re becoming. And you’re not alone.
Sources:
- American Psychological Association – Definition of Trauma
- Duke University Personal Assistance Service – Trauma Symptoms & Causes
- Dr. Gabor Maté – Trauma’s Definition and Impact
- Verywell Health – What Is Trauma? (Ashley Olivine, PhD, MPH, 2024)
- Emotions Therapy (Calgary) – Healing From Childhood Trauma (Rod Mitchell, RP)
- Northeastern University Sci Magazine – Trauma and Resilience
- Crossroads Antigua – Stages of Trauma Recovery (Judith Herman’s model)
- Verywell Mind – Post-Traumatic Growth (Sanjana Gupta, 2023)
- Big Think – Does the Body Keep the Score? (Saga Briggs, 2023)
- Psychology Today – Misusing the Term “Trauma” (Amanda Ann Gregory, LCPC, 2023)
- SAMHSA (NCBI) – Trauma-Informed Care: Impact of Trauma (TIP 57, 2014)
- National Center for PTSD (VA) – Trauma Screening Questionnaire (TSQ) Description.