Trauma can leave survivors feeling overwhelmed by fear long after the threat is gone. It’s easy to assume that emotional trauma is something you should just “get over” once the event has passed. The truth is, trauma can literally change how your brain works, which might explain why you still feel on edge or emotionally numb long after the event. It’s not “all in your head” – trauma leaves an imprint on the brain and body. Thankfully, it’s not a life sentence: experts emphasize that the brain can heal from trauma with the right support. The same neuroplasticity that allowed trauma to rewire your brain now lets it rewire itself in a positive way.
No matter how “mild” or “severe” your traumatic experience, mental health experts say that proactively addressing it is key to recovery. But what if you feel mostly okay and aren’t ready to dig into the past? Are there small steps you can take on your own to help your brain heal? And how do you know if you’re actually getting better, and not just avoiding the pain? Below, we’ll explore what trauma does to the brain, and science-backed ways to help your brain recover, from professional therapies to everyday lifestyle approaches.
What does emotional trauma do to your brain?
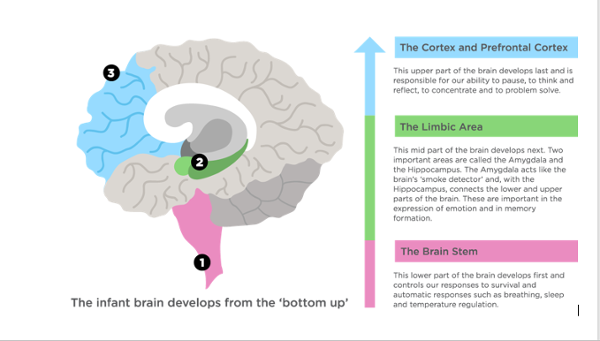
When you experience a traumatic event, your brain’s survival circuitry kicks into high gear. One of the key players is the amygdala – the brain’s internal alarm system. Trauma can make the amygdala hyperactive, so it fires off fear and stress signals even in safe situations. This is why you might feel hypervigilant or easily startled, as if danger is around every corner. Meanwhile, the prefrontal cortex (PFC) – the part of the brain that helps with rational thinking, focus, and impulse control – tends to go offline under extreme stress. A weakened PFC makes it harder to regulate emotions or think clearly, which is why trauma survivors might feel impulsive or struggle with concentration and decision-making.
Another area affected is the hippocampus, the brain’s memory center. Trauma can actually cause the hippocampus to shrink or malfunction, leading to fragmented or intrusive memories. Ever had flashbacks or felt like you were reliving the trauma through nightmares? You can thank those trauma-induced memory changes. On a biological level, a traumatic experience floods your system with stress hormones like cortisol and adrenaline, locking you into fight, flight, or freeze mode. In the moment, this response helps you survive. But if your brain stays stuck in survival mode long after the threat is gone, it can wreak havoc on your mind and body. A constantly overactivated stress response can lead to symptoms like insomnia, irritability, and difficulty concentrating. Trauma literally “reshapes” brain circuits, which helps explain why survivors may develop intense anxiety, emotional numbness, or even explosive anger, along with memory issues and trouble maintaining relationships.
The bottom line is that trauma causes real, physical changes in the brain. It can be validating to know there’s a biological reason for your pain – but also scary to wonder if it’s permanent. The good news is that the brain is incredibly resilient.
Can the brain heal after emotional trauma?
In one word, yes. The human brain has a remarkable ability called neuroplasticity, which means it can change and adapt by forming new neural connections. This is the same mechanism that allowed trauma to change your brain – and it’s also the key to healing. “The brain can heal from trauma… if we know how to help it! Just like a muscle can be strengthened, we can also change our minds,” one brain health coach explains. In other words, with the right interventions and environment, your brain can literally rewire itself in healthier ways.
Bessel van der Kolk, MD, a leading trauma psychiatrist, explains that certain treatments “activate the brain’s natural neuroplasticity to rewire disturbed functioning” and help survivors regain their ability to feel safe and in control, essentially allowing the brain to form new pathways that override the “stuck” trauma responses. As Melisa Sandoval, a trauma-informed educator, puts it, trauma is “not a life sentence.” She emphasizes that the brain can heal “with the right relationships and environment”. Supportive relationships help calm your nervous system, reminding your brain that it’s safe now.
Of course, healing doesn’t happen overnight – and recovery looks different for everyone. But if your brain has been deeply impacted (for example, in PTSD), you might need more guided help to reclaim your life. The journey can involve therapy, self-care, lifestyle changes, or often a combination of all three. The key point is that the brain wants to heal – you just have to give it the right conditions. So, what are those conditions?
Reframing trauma respects the role of memory in shaping identity, unlike erasing it. Neuroscience supports the use of therapy and neuroplasticity to reduce emotional pain without deleting memories, promoting healing and resilience through adaptive integration.
— AP Dr Chia Yoke Yin
Therapies that help rewire a traumatized brain

Talking about the trauma can be hard, but there are several evidence-based therapies designed to help your brain process and move forward. Here are a few approaches experts often recommend to heal the brain:
- Trauma-Focused Cognitive Behavioral Therapy (CBT): CBT helps you identify and change negative thought patterns that keep you stuck in trauma. For instance, survivors often carry beliefs like “I am unsafe” or “It’s my fault.” In CBT, a therapist works with you to challenge and reframe these thoughts into healthier ones. This isn’t just “positive thinking” – brain imaging studies show that CBT can actually reduce overactivity in the amygdala (meaning fewer false alarms of danger) and enhance the prefrontal cortex’s ability to regulate emotions. CBT can help calm an over-alert brain and teach it new, healthier ways to interpret the world.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is a unique therapy where you recall aspects of the traumatic memory while doing guided bilateral stimulation (like following a moving light with your eyes). Research shows EMDR can be highly effective for resolving trauma. The process helps the brain reprocess traumatic memories and store them more like ordinary memories. Studies find EMDR not only reduces PTSD symptoms but also strengthens connections between the brain’s emotional center and its logical thinking center – essentially helping your amygdala and prefrontal cortex communicate better. Many people say that after EMDR, the traumatic event feels more distant and less painful – a sign that the brain has finally moved it into the past.
- Somatic Therapy (Body-Focused Healing): Trauma isn’t just in your head – it’s also stored in your body (think tense muscles or a racing heart). Somatic therapies (like Somatic Experiencing, sensorimotor therapy, or trauma-informed yoga) help release that pent-up energy and teach your body to feel safe again. As one renowned expert put it, trauma victims “cannot recover until they become familiar with and befriend the sensations in their bodies”. Gently working through bodily sensations in this way lets the fight-or-flight energy finally discharge, calming your nervous system in ways that talk-only therapy might miss.
Lifestyle habits to help your brain heal

Therapy is important, but what you do in daily life also has a huge impact on healing your brain. Every day is an opportunity to reinforce either the patterns of trauma or the patterns of recovery. Here are some science-backed lifestyle strategies that support brain healing and resilience:
- Mindfulness & Meditation: Practicing mindfulness (staying present and non-judgmentally aware) can literally help rewire your brain after trauma. Regular meditation is shown to shrink an overactive amygdala and strengthen the prefrontal cortex (helping you stay calm and focused). It also lowers cortisol, the stress hormone, which is often elevated in trauma survivors. Even a few minutes of deep breathing or mindfulness each day teaches your nervous system to relax.
- Physical Exercise: Exercise is one of the best natural ways to heal the brain. Aerobic activities like running, swimming, or dancing release endorphins – your brain’s feel-good chemicals – which boost your mood and reduce anxiety. Physical activity also boosts brain-derived neurotrophic factor (BDNF) – a protein that helps repair and grow brain cells. (Think of BDNF as fertilizer for your brain, helping new neural connections sprout.) Studies have found regular exercise can sharpen memory and thinking, while also reducing symptoms of anxiety and depression. You don’t need to become a marathoner – even daily walks or yoga can yield benefits. The key is consistency: moving your body consistently helps move your brain out of trauma mode.
- Healthy Diet: Nutrition plays a role in brain recovery too. An anti-inflammatory, balanced diet gives your brain the building blocks it needs to heal. For example, omega-3 fatty acids (found in fatty fish, flaxseeds, walnuts) are known to support brain health and may help with mood regulation. Antioxidant-rich foods (berries, greens, colorful veggies) help combat oxidative stress in the brain. Simply put, feeding your body well can improve your overall mental resilience.
- Prioritize Sleep: Sleep is when your brain does a lot of its healing work. Deep sleep, in particular, is when memories get processed and emotions get sorted out. During deep sleep your brain can integrate traumatic memories and make them less intense and charged. Aim for a consistent sleep schedule and a relaxing pre-bed routine to help your brain wind down. Getting decent sleep is one of the most restorative gifts you can give your brain.
- Social Support: Positive social connection is like medicine for a traumatized brain. Spending time with supportive people lowers stress and even releases oxytocin, the “bonding” hormone that counteracts stress. If trusting others is hard after trauma, that’s understandable – but even one trusted friend, family member, or support group can remind you that you’re not alone, which greatly aids recovery.
Embracing the healing process
Recovering from emotional trauma is challenging, but it’s possible. Your brain is not broken – it’s adaptable and capable of recovery. With the right help and habits, those trauma-related brain changes can be softened or even reversed. Along the way, be kind to yourself. Healing often isn’t linear. Be patient and watch for small signs of progress – maybe you’re sleeping better, feeling less on edge, or starting to regain hope. These little wins are all signals that your brain is healing.
If you’re a trauma survivor, know that you’re not alone and that help is available. Consider reaching out to a trauma-informed therapist, leaning on a trusted friend, or joining a support group. Build daily routines that nourish your mind and body. Over time, the new neural pathways you cultivate will grow stronger, and the old trauma pathways will fade.
Healing the brain after emotional trauma may take time, but it does happen. Step by step, with therapy, self-care, and support, your brain can rebuild and renew itself. You deserve to feel safe, whole, and hopeful again.
Sources:
- Sabino Recovery – How trauma affects the brain & body
- Insights Psychology (2025) – How Trauma Shapes the Brain & Pathways to Recovery
- Insights Psychology – Evidence-Based Strategies for Trauma Healing
- PsychCentral – Neuroplasticity and Healing from Childhood Trauma
- PACEs Connection – Trauma is not a life sentence
- Khiron Clinics – What Is Neuroplasticity, And How Can It Help In Recovery?
- Bessel van der Kolk, MD – The Body Keeps the Score
- A Place of Hope – The Role of Sleep in Trauma Recovery
- Bessel van der Kolk (Goodreads quote) – Befriending the body

